
Our Research Areas
Cardiovascular Risk Reduction
The Global Burden of Disease study estimate of age-standardized cardiovascular death (CVD) rate of 272 per 100 000 population in India is higher than the global average of 235 per 100000 population. Diabetes, hypertension and dyslipidemia are the major modifiable risk factors of CVD. The prevalence of diabetes is reported to be 15%, hypertension 28% and dyslipidemia 79%. Co-existence of hypertension in patients with diabetes is reported to be 59.5% and dyslipidemia 50%, while the prevalence of hypertension and dyslipidemia among patients with diabetes is approximately 51% and 61%.
Currently individual cardiovascular risk factors i.e. diabetes, hypertension and dyslipidemia are managed individually and lower the cardiovascular risk up to 20%–30%, however, substantial residual risk still persists with clinical and economic consequences. CV risk factors tend to occur as a cluster and the relationship between the CV risk factors is synergistic. Treatment guidelines have recognized that multifactorial treatment approach is required to address all risk factors and recommend to use all risk assessment charts to tailor each patient’s risk profile.2 This has resulted in a shift from management based solely on single risk factor, towards managing a patient’s total CV risk.
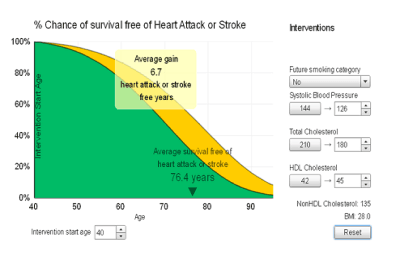
Our approach is based on total risk management by simultaneously improving the key risk factors i.e. dyslipidemia, diabetes and hypertension. Besides, a lifetime approach to CV risk is important since both CV risk and prevention are dynamic and continuous as patients age and/or accumulate co-morbidities. Hence, a CV risk score which will predict lifetime risk based on reduction in multiple risk factors i.e., blood pressure and non-HDL while also accounting for predicted risk in the context of competing risks from other diseases over the remaining expected lifespan will help in identifying high-risk individuals both in the short and long term and treating them.
Cardiovascular & Metabolic Diseases: Diabetic Complications
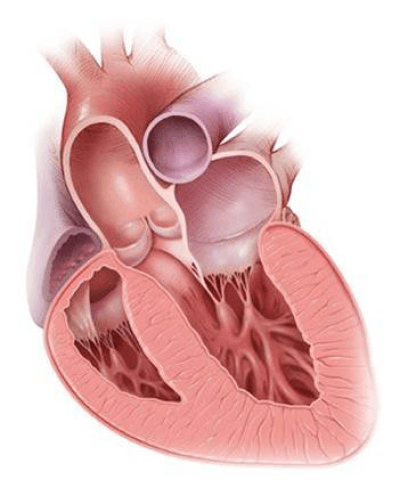
Diabetes is a condition that is prevalent in about 5-7 % of the adult population. Prolonged and high blood glucose is now recognized as a primary cause of diabetic complications. There has been considerable progress in the sphere of glycaemic control, nevertheless, the prevalence of the complications is still around 20% in patients who have had diabetes of 5 years or more. These pose a significant social and economic burden to patients and healthcare system. More than 60% of the cost of managing diabetes stems from the cost of hospitalization for the complications of diabetes. Among patients with diabetes, heart failure is known to have a worse prognosis even after adjusting for other cardiovascular (CV) risk factors and Ischemic Heart Disease, the 5 year mortality being close to 50%.
The maladaptive cardiac remodeling associated with diabetes with preserved ejection fraction remains an unmet need due to unsatisfactory diagnosis and also management because of lack of effective pharmacological targets to improve outcomes. The emphasis in the management and prevention of heart failure with preserved ejection fraction is shifting to the control of consequences of diabetic hyperglycemia itself. Independent of underlying renal function, diabetes also has an adverse impact on outcomes in diastolic HF.
We are focusing this unmet need by working on mechanisms that retard the progression of and reverse diabetic heart failure by inhibiting the pathways involved in altering protein structure and function in diabetic state and the ensuing inflammatory cascade.
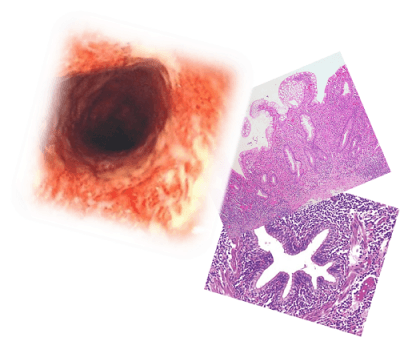
Inflammation: IBD COPD Asthma
Inflammatory response generally initiates by signals set-off by pathogen invasion or tissue injury. This, in turn, initiates the activation of intracellular signalling cascades and subsequently results in increased expression of proinflammatory pathways. When these responses persist despite resolution of the initial insult, these processes can become pathological. A wide spectrum of human diseases are associated with chronic inflammation and number of drugs have been used for the treatment of these inflammatory diseases. However, there still remain unmet needs due to several reasons and several limitations. Many current therapies are non-selective and associated with significant side effects limiting their tolerability. Furthermore, many patients become unresponsive to these first-line therapies.
Chronic inflammatory diseases, such as inflammatory bowel disease (IBD), chronic obstructive pulmonary disease (COPD) and asthma, pose a significant global economic and public health burden. Dysregulated immune responses underlie the disrupted homeostasis at mucosal barrier sites in the intestine and lungs in these conditions. We continue to search for new ways of addressing these unmet needs with advancing of our knowledge of the inflammatory pathways and their role in the pathophysiology of conditions.

